Introduction to Insurance Credentialing
Navigating the complex world of insurance credentialing can be quite challenging for psychiatric mental health nurse practitioners (PMHNPs). However, obtaining credentials is a vital step in establishing your practice, as it enables you to accept insurance payments and provide more affordable services to your patients. In this comprehensive guide, we will walk you through the credentialing process for various insurance carriers, including Medicare and Medicaid MCO plans. By following these steps, you can lay a solid foundation for a successful PMHNP practice.
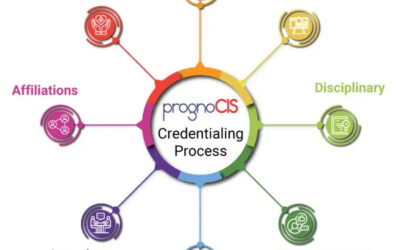
Understanding the Credentialing Process
Insurance credentialing is a thorough procedure that involves verifying a healthcare provider’s qualifications, education, and experience to ensure they meet the requirements set forth by insurance carriers. The ultimate goal of credentialing is to guarantee the highest quality care for patients.
Step by Step: Insurance Credentialing for PMHNPs
To make the process more manageable, we have broken it down into a series of steps:
Prepare Your Documentation
Before initiating the credentialing process, gather all necessary documents, including your resume or CV, state nursing license, DEA registration, malpractice insurance, and any relevant certifications. Having these documents ready will help streamline the process and prevent delays.
Choose the Insurance Carriers
As a PMHNP, you’ll need to decide which insurance carriers you want to work with. Some of the most common carriers we credential for include:
- Aetna
- Blue Cross Blue Shield
- Cigna
- Humana
- UnitedHealthcare
- Medicare
- Medicaid MCO plans (such as Amerigroup, Molina Healthcare, and WellCare)
Keep in mind that credentialing with multiple carriers will expand your patient base and increase your practice’s revenue potential.
Complete the CAQH ProView Application
The Council for Affordable Quality Healthcare (CAQH) ProView is an online database widely used by insurance carriers to access provider information during the credentialing process. Completing your CAQH ProView profile is a crucial step, as it simplifies the submission process for multiple carriers.
Submit Applications to Insurance Carriers
Once your CAQH ProView profile is complete, submit your credentialing applications to the chosen insurance carriers. Each carrier may have its unique application process and requirements, so be sure to carefully follow their instructions.
Monitor the Credentialing Process
The credentialing process can take anywhere from 60 to 180 days, depending on the carrier. During this time, it’s essential to stay proactive and follow up with carriers to check the status of your applications. Being proactive can help prevent delays and expedite the process.
Finalize Your Contracts
Once you receive approval from the insurance carriers, review and finalize your contracts. Pay close attention to the reimbursement rates, billing guidelines, and other essential contract terms.
Update Your Practice Information
After completing the credentialing process, make sure to update your practice information on your website, marketing materials, and online directories to reflect your new in-network status with the insurance carriers.
How BillMed Can Help with Your Credentialing Process
At BillMed, we understand that the credentialing process can be time-consuming and complicated for busy PMHNPs. That’s why we offer a full suite of credentialing services designed to streamline the process and help you focus on what matters most – providing exceptional care to your patients.
Our experienced credentialing team will:
- Guide you through the entire credentialing process, from gathering necessary documentation to submitting applications and monitoring their progress.
- Help you choose the right insurance carriers for your practice, ensuring that you’re in-network with the carriers that best suit your needs and patient population.
- Provide expert assistance in completing your CAQH ProView profile, ensuring that your information is accurate and up-to-date.
- Assist with contract negotiations, helping you secure favorable reimbursement rates and contract terms.
- Offer ongoing support to help you maintain your credentials and stay in-network with your chosen carriers.
Additionally, we offer By partnering with BillMed for your credentialing needs, you can rest assured that you have a knowledgeable team by your side, ready to help you navigate the complexities of the credentialing process. Let us help you unlock your PMHNP practice’s full potential and provide the exceptional care your patients deserve.
Conclusion
Insurance credentialing is an essential aspect of establishing a successful PMHNP practice. By following this comprehensive guide and partnering with an experienced credentialing team like ours at BillMed, you can streamline the process and focus on providing exceptional care to your patients. With the right approach and support, you’ll be well on your way to unlocking your practice’s full potential.